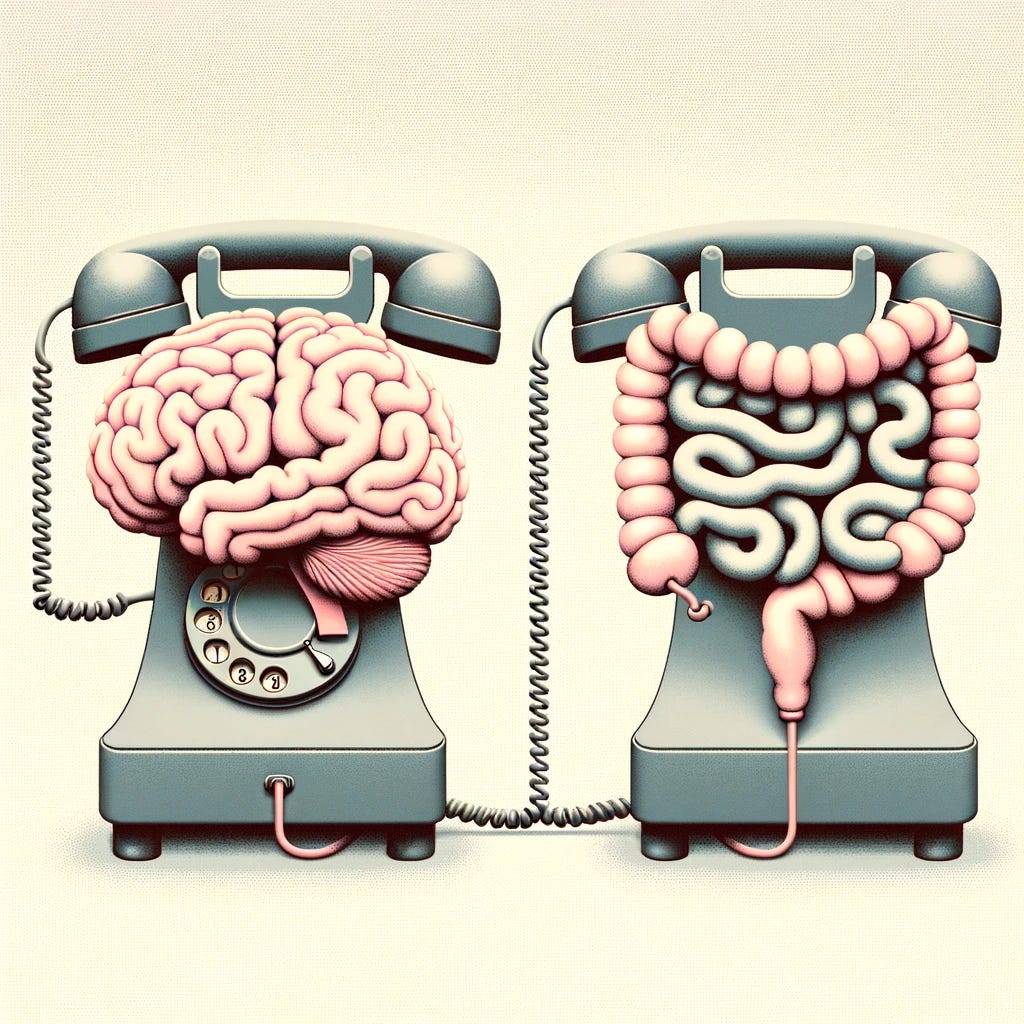
The Gut-Brain-Axis: An Intro (Part 1)
What is it, how do we know the gut and the brain are connected, how do the gut and brain interact in mental health
Firstly, what is the gut-brain-axis?
The gut-brain-axis (or GBA) is the network by which the gut and the brain communicate with each other (more on the mechanics of this later). Of course, this is not a new concept. We’ve known for many years that communication between the two is taking place. For example, when we’re about to eat, our brain sends messages to our digestive system to get ready, and when we’re full, our gut sends messages to our brain to stop eating. The new and exciting bit is the link between the bacteria in our guts, the gut microbiome, and the brain, and particularly our mental health. To recall our blogpost on the gut microbiome, this is the trillions of microbes (mainly bacteria but also viruses, fungi etc. that live in our guts).
OK, so how do we know that gut bacteria and mental health are connected?

Over a decade ago, a team of researchers took faecal matter (yes, that is what you think it is: poo), from people with depression and transplanted it into healthy rats, moving gut bacteria from unhealthy donors to healthy recipients. These rats then started displaying behaviours associated with depression(!) like avoiding pleasurable activities. This was the first strong evidence that gut bacteria could be linked to mental health. Of course, this was a study in animals, so we’d need more evidence of this in humans before we read too much into it, even though these studies are going strong.
In humans, there are ethical questions about transplanting faecal matter that might potentially give people depression to discover something, so we went about it differently. Scientists soon discovered, via new DNA sequencing technologies, that the gut bacteria of a depressed person is significantly different to that of a healthy person (see this paper for a review). This strengthened the idea that gut bacteria and mental health were linked, and this time with human evidence. Even stronger evidence of this came from cases where faecal matter transplants for people with gastrointestinal issues also treated their co-occurring depression. This has since been validated a number of times in both mice and humans. On top of that, a number of studies have given people with anxiety and depression bacteria in the form of probiotics, and have shown improvements in patient symptoms. This is potentially game changing for mental health. Not only do we better understand these disorders but studies like these could open up whole new avenues for treatment. The next question we needed to answer, was how. How is it that bacteria in the gut are affecting the brain and our mental health?
Makeup of the GBA
Before we answer that question, let’s break down some of the biology in the GBA (note, we’re keeping it simple to avoid going into a full biology lesson)
1. First we have the aforementioned gut microbiome and the trillions of bacteria it houses across the intestines. These bacteria in the gut break down food and produce chemicals known as metabolites (i.e. the outputs of metabolism). These metabolites support a huge range of functions which are necessary for optimal brain functioning and mental health.
2. Up next is the immune system. The immune system is responsible for protecting our bodies from things like infection and 70% of it is based in our guts. This makes sense as our mouth is one of the main ways that harmful stuff can get inside us and cause damage. The immune system’s go to response in terms of detecting potentially harmful stimuli is inflammation. Turns out inflammation plays an important role for mental health.
3. Third, is the vagus nerve, a large nerve that runs from the brain through the entire digestive system up to the colon. It is the primary highway for communication between gut and brain. It’s likely that whatever signals are going up and down this nerve are important for mental health.
4. Finally, we have the brain. A hugely complex organ which is responsible for a huge amount of our functioning and of course implicated in all mental states and disorders associated with mental health.
Mechanisms of gut-brain-mental health interaction
How the gut and brain talk to each other in the area of mental health is still under heavy research, and so, many of the answers to our questions are simply, ‘we don’t know yet’. But here are a few ways that research has begun to illustrate the gut affecting mental health:
1. A healthy gut promotes a healthy brain - a healthy and functioning microbiome will be producing the necessary metabolites for a healthy brain and body. For example, bacteria including Enterococcus and Streptococcus species are responsible for producing serotonin in the gut. Although gut serotonin cannot pass through the barrier around the brain, it can still stimulate the vagus nerve which connects the gut and brain, and is necessary for optimal functioning. Since serotonin is one of the main neurotransmitters involved in depression, a disrupted microbiome means reduced serotonin production and interrupted signalling to the brain.
2. An unhealthy gut creates an unhealthy brain - when the bacteria in the gut are dysregulated, we don’t just lose the benefits of what they used to do when in a regulated state. There’s evidence that the bacteria can also facilitate states in the brain that promote mental health disorders. One example is tryptophan, an amino acid we get from eating eggs, meat, oats, and other foods. This is used to make the aforementioned serotonin inside the brain where it plays an important role in happiness. However, where we have a disrupted gut microbiome, instead of being converted into serotonin and promoting happiness, it now gets converted to something called indole-3-aldehyde which can cause inflammation in the brain. This brain inflammation has also been linked to depression.
3. Triggering of the immune system in the gut - the immune system is separated from the gut by a layer of mucus. This prevents the immune system from responding to anything in our guts that’s just passing through. A healthy microbiome is necessary to maintain this mucus lining. Where the microbiome is disrupted, the lining breaks down and more things can set off the immune system triggering inflammation. This is sometimes referred to as leaky gut syndrome. This chronic inflammation has been linked to mental health disorders.
Wrapping it all up
Within GBA research it’s now assumed that the bacteria in the gut and the brain are connected. We understand the main elements involved (bacteria, vagus nerve, immune system etc.) but the mechanics are still being discovered. Despite the early stage of this research we already have some clues as to how these two interact and therefore what we might want to do to boost the GBA’s health when it comes to mental health disorders. We cover this in part 2 of this series!